|
Rotation Policies & Procedures
Night Float
Last Updated: 03/23/20
I. Guidelines and Policies
II. Rotation Logistics
I. Guidelines and Policies General Policies
A. Admitting Residents
- Overview
- Two night float residents will be designated as admitting residents each night. Each resident will carry an admission pager and their personal pager
- Residents will arrive at 6:30PM to begin overnight admissions.
- Admitting residents may be asked to come in earlier by crosscover resident if long call teams receive all admissions prior to 6:30PM
- Admissions Workflow
- ED Admissions
- ED resident/attending will place bed request to unassigned team once decision has been made to admit patient.
- SPPO will update order to appropriate team and attending, and page night float resident to notify them of admission
- At start of shift, admitting residents should notify SPPO which team overnight admissions will begin with.
- Admissions generally begin with team with lowest census, and go alphabetically, though process can be modified at discretion of admitting residents
- Residents will call ED within 15 minutes to obtain signout for patient. Once signout is complete, admitting resident will assume full responsibility for patient
- Resident should determine if patient is a Family Medicine continuity patient before calling for signout to avoid unnecessary transitions of care.
- Residents will alternate with admissions over course of night, as appropriate.
- SPPO will automatically assign patients alphabetically in drip as admitted. Admitting residents should notify SPPO of any reassignments (e.g. if bounceback or team caps, see below) to ensure admission log is correct.
- Prior to end of shift, admitting resident should inform SPPO which team daytime admissions will begin with
- First team to receive daytime admission should be based on overnight admissions and proceed alphabetically. E.g., if teams A, B, C and D are admitting, and team A receives last admission overnight, team B will receive first daytime admission, then C, D, etc.
- Admitting residents will accept last overnight patient at 6:00AM, to allow sufficient time to complete admissions and prepare for signout
- If any admissions are received after 6:00AM, admitting residents should notify ED that day team will call back for signout. Day team should be notified of any pending admissions during signout.
- At end of shift, admitting resident will sign out all admissions to day teams. Entire team, including senior resident, should be present for signout.
- Admitting resident should provide succinct signout for all patients, in particular focusing on any significant findings, pending labs/imaging, patient acuity etc.
- Outside Hospital Transfers
- All outside hospital transfers are coordinated through the Transfer Center, and require acceptance by a hospitalist. All patients accepted for transfer will be listed on SharePoint
- SPPO will assign OSH transfer patients as part of drip. Patients may be assigned to team before they physically arrive at UCI. Patients should be kept on the team they were assigned, regardless of when they arrive.
- If patient does not arrive prior to 6:00AM, admitting resident should place initial admission orders and start H&P. Patient should be signed out to day team to complete admission once patient arrives.
- Transfer Center (x2222) may be able to provide records sent from OSH to assist with starting admission for patients who do not arrive overnight.
- MICU/CCU Transfers
- SPPO will assign MICU and CCU patients will be assigned to ward teams as they are assigned beds overnight.
- All patients assigned overnight will be cross-covered by MICU team.
- All MICU/CCU transfers should be noted on admission log. Day teams should be notified at signout of any transfers; day team will contact MICU/CCU to obtain signout on these patients.
- CDDC/GI Admissions
- Patients may be transferred from CDDC observation unit overnight if their 47hr observation time will expire before they are stable and ready for discharge
- 47hr observation time begins from time patient is brought to CDDC prior to procedure, NOT following procedure
- CDDC nocturnist should place transfer orders and sign out to admitting resident any patients being transferred to hospital. Admiting resident will only assume care for patient once physically transferred from CDDC.
- Admissions Requirements
- All admissions to wards require the following:
- Complete H&P
- All patients require a complete H&P, with documentation of succint HPI, relevant past medical, surgical, family and social history, review of systems, focused physical exam, and problem-based assessment and plan
- H&Ps should be assigned to attending on the following day for cosignature
- Admission Orders
- Admission orders can be placed using "GEN IP General/Non-ICU Order Set" in EPIC
- Order set includes admission order with designation of team, attending and level of care.
- Level of care designation is determined by ED based on their initial evaluation. If, following evaluation, resident feels higher level of care is needed, e.g. telemetry vs. med/surg, SPPO should be notified immediately to ensure appropriate bed assignment
- Medication Reconciliation
- All patients should have medication reconciliation completed on admission following discussion with patient and/or family
- ED or floor nursing can assist with entering home medications if not present in EPIC
- VTE Prophylaxis Assessment
- All patients should be assessed for appropriate mechanical or chemical VTE prophylaxis on admission based on VTE and bleeding risk. Prophylaxis should be ordered through admission order set
- If VTE chemical prophylaxis is not ordered, reasoning should be documented in H&P.
- Code Status Documentation
- Code status should be documented for all patients following discussion with patient. If patient unable to participate in code discussion, attempt should be made to discuss with DPOA or locate POLST to appropriately document code status.
- Day team should be notified at signout of any patients for whom code status is unclear.
- Caps and Patient Distribution UPDATED
- Overnight, all uncapped ward teams will be open for new admissions
- Night float residents will assign admissions (including ED admissions, outside hospital transfers, and MICU/CCU transfers) in usual drip fashion
- Drip will begin with one of the teams that is admitting the following day, and proceed in alphabetical order through the other admitting teams. No call teams will be the last to receive admissions. E.g. if on the following day ...
| ... teams A, B, C, D admitting: |
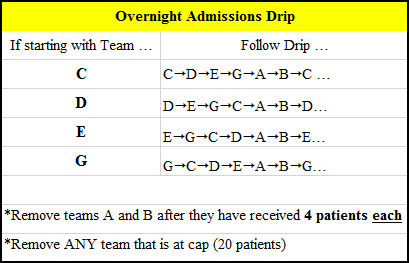 |
| ... teams A, B, E, G admitting: |
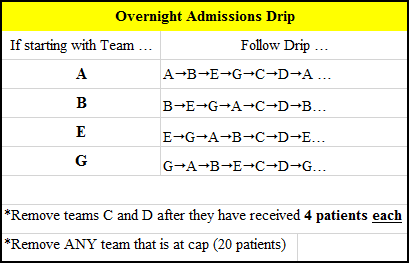 |
| ... teams C, D, E, G admitting: |
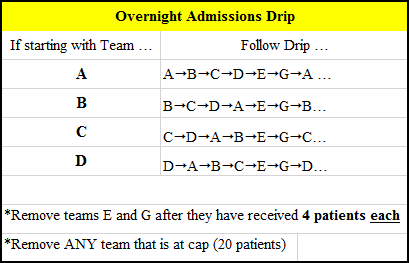 |
- Decision on which team receives first admission overnight at discretion of night float residents based on team censuses
- No call teams will receive maximum of 4 new admissions per team. Once no call teams have reached limit, they will be taken out of the drip.While night float residents are not required to triage admissions, the following types of patients should preferentially be assigned, if possible, to teams where a senior resident will be present:
-
- Patients admitted to Stepdown level of care
- Patients transferred from outside hospital for higher level of care
- Patients transferred to floor from Intensive Care units
- Patients deemed to be higher risk for decompensation, based on admitting resident's clinical judgment
- To facilitate even distribution of patients between teams, "soft" cap of 18 patients will be eliminated. All teams will cap at 20 patients.
- Bouncebacks
-
- Resident Bouncebacks: Bouncebacks follow senior resident and should be readmitted to original team except:
- If it is the first or last day of the block
- If team is not admitting (no call) and senior resident is not present. Patient should be assigned to admitting team (for credit), and transferred back to original team the following day (without credit)
- Team may still accept bouncebacks on days they are no call if senior resident is present
- NP Bouncebacks: Bouncebacks primarily cared by NP can be accepted by original team regardless of call status or presence of senior resident. These patients will be managed by NP and attending physician.
B. Crosscover Resident
- Overview
- One night float resident will be designated as crosscover resident
- Crosscover resident will carry three pagers: crosscover pager, Team H pager (will also receive RRT/code blue pages), and personal pager.
- Night float resident will arrive at 5:00PM to begin cross-covering and assign long-call admissions (see below).
- Crosscover Workflow
- Ward Patient Cross-coverage
- Crosscover resident will arrive at 5:00PM. On arrival, resident should locate and turn on three pagers: 1) crosscover pager, 2) Team H pager, and 3) admission pager (will be handed off to admitting residents at 6:30PM)
- Resident will receive signout from no and short-call teams at 5:00PM, and long-call teams at 7:00PM
- Resident should obtain succinct, though thorough signout from teams. Particular focus should be paid to any unstable or sick patients, specific tasks to follow up on, and anticipatory guidance for any expected issues.
- Once signout is received from all teams, resident will note censuses and attendings on admission log (in binder).
- Resident will follow up on any cross-cover "to-do's"
- Resident will respond to all nursing pages within 15 minutes. Any issues will be noted for signout to day teams in morning
- Any signficant issues, e.g. RRT/code blue/airway emergency, change in code status, AMA discharge, etc., should be documented in Event Note in EPIC.
- MICU patients will be cross-covered by the respective night float depending on patient's location at time of ward signout (5:00PM)
- If patient is transferred out of MICU before 5:00PM, ward crosscover resident will cross-cover patient
- If patient is transferred out of MICU after 5:00PM, MICU night float team wil cross-cover patient
- MICU night float team will signout any events to ward team, if applicable
- Resident will signout to teams in AM. Signout should, in particular, focus on any significant events, pending labs/imaging, etc.
- Long Call Admissions Assignment UPDATED
- Crosscover resident will be responsible for assigning long call admissions, including from ED, OSH transfer, or MICU/CCU, to teams from 5:00-7:00PM
- At start of shift, resident should notify SPPO which team will receive first admission of long call.
- Generally, team that received earlier admission during day will receive first long call admission. E.g. if team C received last day admission at 3:00PM, and team D received last admission at 4:30PM, team C will take first long call admission. However, assignment is at discretion of crosscover resident
- Long call teams will admit up to 3 patients until 7:00pm, or until they reach cap.
- MICU transfers assigned during long call will be cross-covered by respective night float depending on patient's location at 5:00PM (see above)
- All admissions will be paged by SPPO to admission pager
- Team H Consults
- Crosscover resident will carry and receive consults via Team H pager overnight
- Night float resident will clarify with primary service resident if recommendations are required overnight ("Urgent Consults") or can be seen by daytime residents following day ("Non-Urgent Consults")
- Urgent Consults
- Flex resident will see and evaluate all urgent consults, e.g. preop evaluation for urgent surgery, time-sensitive questions, as soon as possible after receiving consult
- Resident will staff all preoperative evaluations for hip fracture patients with the medicine nocturnist (effective March 2020)
- Resident will staff all other urgent consults with on-call attending (p2112). Shoud the on-call attending feel that hte patient needs to be seen urgently overnight, they should communicate with the medicine nocturnist to assist
- Non-Urgent Consults
- Resident will obtain basic signout (patient info, primary service, consult question) from primary service resident
- Resident will forward details to both daytime Team H residents of pending consult and place patient on Team H team list
- To add patient to Team H list:
- Find patient in EPIC
- Right click on patient, and click "Treatment Team"
- Enter "Hospital" under "Name" and click Search
- Double click *Consult* Hospital Medicine and click "Accept"
- RRT/Code Blue Team
- Crosscover resident will respond to all RRT and code blue emergencies overnight along with MICU night float resident
- Either crosscover or MICU resident will be responsible for documenting RRT/code blue details in EPIC
Service Agreements & PoliciesCriteria are summarized below for each respective service. For additional details, please see full service agreement (located under "Policies" on residency website)
A. Family Medicine
Last Updated: 02/06/2019
- Admission Criteria
- In order to be admitted to Family Medicine service, patients must be ALL of the following criteria
- Patient identifies a UCI Family Medicine or Geriatrics provider as their primary provider, and intends to follow up on discharge from hospital
- Patient has been seen for at least 2 visits during the previous 2 years by 1) any Family Medicine resident, 2) Family Medicine provider, or 3) Geriatrics provider at their outpatient clinic site (FQHC Santa Ana, FQHC Anaheim, Gottschalk Medical Plaza, UCI Senior Center, PACE clinc (if attending is FM faculty)
- These two visits are to be continuity visits (not just urgent urgent care)
- To avoid disruption in continuity of care, patients should not be transferred between services after day team has acquired the patient.
- Family Medicine/Geriatrics providers include:
| Arghami, Elham MD |
Arroyo, Jeff MD |
Austin Rachel |
Biddy, Edna MD |
| Centanni, Leah |
Craemer, Elana MD |
Deshpande, Prajakta MD |
Doloulei, Reza MD |
| Dow, Emily MD |
Gibbs, Lisa MD |
Haq, Cynthia MD |
Khalighi, Katayoun MD |
| Kilgore, David MD |
Kim, Brian MD |
Kroner, Christopher MD |
Larsen, Kathyrn MD |
| Mayorga, Jose MD |
Morohashi, David MD |
Nguyen, Tan MD |
Prislin, Michael MD |
| Raymundo, Marianita MD |
Salcedo, Betzy MD |
Seghal, Sonia MD |
Suskin, Shea MD |
| Tam, Steven MD |
Tran, Huy DO |
Vadecha, Nina MD |
Valerie George, PA-C |
| Vega, Charles MD |
Vo, Baotran, MD |
Whalen, Megan |
- Caps
- Capped at 15 patient (including pediatrics and OB)
- Once the cap above is hit for the FM service, the next patient with a senior health center PCP will go to Internal Medicine service and the next patient with a PCP at the FQHC will go to Family Medicine service.
- Once FM hits 15 adult patients, then all patients will go to the IM teams until the FM team uncaps. If all teams are capped above 15 then everyone will share the overflow and continue to take admissions.
- Overflow Policy
- In event all IM admitting teams are at or above 18 patients, FM will assist with admissions as below:
- If FM uncapped: Service will get inserted into drip and take both Medicine and FM patients
- If FM and IM capped:
- FM will admit all FQHC-Santa Ana/Anaheim patients
- IM will admit all Senior Health Center patients
|
B. Cardiology
Last Updated: 11/15/2018
- Admission Criteria
- Cardiology Service (CCU or Telemetry)
- Newly identified acute heart failure decompensation without other acute noncardiac medical problems
- NYHA class III-IV heart failure considered having high in-hospital mortality (BUN>43, SBP<115, and serum Cr>2.75 (excluding patients with CRF or on hemodialysis))
- Suspected or diagnosed acute coronary syndrome (unstable angina, acute myocardial infarction, aborted sudden cardiac death)
- Newly identified and/or potential life-threatening symptomatic arrhythmia (sustained ventricular tachycardia, high-grade atrioventricular block, symptomatic atrial fibrillation, persistent symptomatic brady- or tachyarrhythmia
- Acute decompensated heart failure requiring or at risk of requiring invasive ventilatory support
- Cardiogenic shock or otherwise requiring chemical or mechanical circulatory support (dopamine, dobutamine, milrinone or adrenergic agonist drip, IABP counterpulsation, LVAD)
- Patient regularly followed by member of Cardiology department and without other acute noncardiac medical problem.
- "Regularly followed" defined as two clinic visits within last 12 months
- "Without other acute noncardiac medical problem" defined by best clinical judgment and decision of ED attending
- Medical ICU Service
- Multisystem organ failure
- Requiring or at risk of requiring invasive ventilatory support, excluding acute decompensated heart failure
- Hospital Medicine
- Acute decompensated heart failure not meeting any of above admission criteria, with Cardiology Nurse Practitioner consult
- Following patients, with consideration for urgent Cardiology consultation:
- Persistent or worsening symptoms despite aggressive and sustained intervention.
- Diastolic dysfunction of unclear etiology.
- Inodilator or vasodilator infusion with worsening of heart failure.
- Suspected acute coronary syndrome (i.e. unstable angina, acute myocardial infarction, aborted sudden cardiac death, unexplained abnormal cardiac enzymes).
- Suspected significant coronary artery disease who are candidates for diagnostic angiography/percutancous or surgical coronary intervention.
- Abnormal provocative stress-test who are candidates for diagnostic angiography/percutaneous or surgical coronary intervention.
- Undergoing evaluation for or post cardiac transplant
- Newly identified serious arrhythmias (e.g. ventricular tachycardia, symptomatic brady or tachyarrhythmias, high grade a-v block).
- Destabilized chronic/known arrhythmias.
- Implanted mechanical devices (e.g. LVADs).
- Implanted electrical devices that require interrogation or are suspected of malfunction (e.g. pacemaker, AICD)
- Candidates for cardiac resynchronization (i.e persistent symptoms + EF <35% + QRS interval > .12 sec).
- Currently regularly followed by a member of the Cardiology department (as defined above)
- For evaluation for transfer to Cardiology service
- Readmission/Bouncebacks
- Heart failure patients readmitted within 30 days should be readmitted under the previous team unless condition requires different admission services as best decided by clinical judgment of ED attending
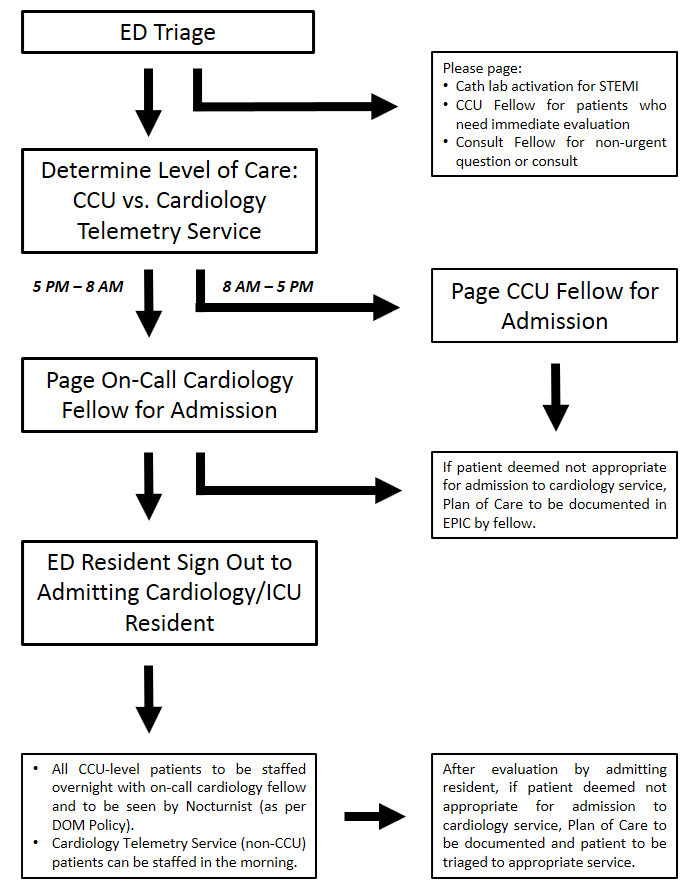
- Admission Workflow
- ED resident will evaluate patient for possible admission to Cardiology service (including both telemetry and CCU level of care) based on Cardiology admission criteria (see below).
- ED resident will contact appropriate Cardiology fellow for acceptance to Cardiology service. Medicine residents cannot accept patients to Cardiology service, and should not be contacted prior to approval from fellow
- 8AM-5PM: CCU Fellow
- 5PM-8AM: On-Call Cardiology Fellow
- Once Cardiology fellow has accepted patient to Cardiology service, ED resident will contact admitting Medicine resident for signout.
- Any patients deemed not appropriate for admission to Cardiology service by fellow will require Plan of Care documentation in EPIC, with further recommendations, if appropriate.
- For daytime admissions:
- Patients will be staffed with daytime Cardiology service attending per usual schedule
- For overnight admissions:
- Admitting Medicine resident will contact on-call Cardiology fellow to staff all CCU level admissions
- Non-CCU (telemetry) level patients may be staffed by primary team in the morning. However, residents are encouraged to contact on-call Cardiology fellow with any questions that arise.
- Nocturnist will also see all CCU level patients per Department of Medicine policies
|
C. Hematology/Oncology
Last Updated: 03/28/2017 Team L Policies
- Admission Criteria and Policies
- Patients with established diagnosis of hematologic malignancies (categories listed below) on active treatment for their neoplasm:
- Any Acute Leukemia, Myelogenous or Lymphoblastic (AML or ALL respectively
- Chronic Myelogenous Leukemia
- Chronic Lymphoid Leukemia
- Lymphoma (Hodgkins or Non-Hodgkins)
- Multiple Myeloma
- Myeloproliferative Neoplasms (for example P. Vera)
- Myelodysplastic Syndromes (for example, myelofibrosis)
- Patients with established diagnosis of hematologic malignancies but admitted for reasons other than receiving anti-neoplastic therapy will be admitted to the Hospitalists service(s) and followed by the consult service (Team S, see below).
- Team L will have a cap of 16 patients until further notice
- Direct admissions, admissions through the ED, and transfers from other services require the notification of and approval of the Team L attending.
- No patient will be transferred to Team L without the express consent and agreement of the Team L attending.
- Neuro-Oncology Primary CNS lymphoma patients will be on Team L only if receiving active anti-lymphoma treatment. Other neurologic oncology patients and neuro-oncology primary CNS lymphoma patients not receiving treatment will be on admitted to Neurology.
- Admissions occurring (arriving on the floor) between 7:00 AM and 5:00 PM will be admitted by one of the advanced practitioners (APs) on Team L.
- Admissions occurring outside of the above time period will be admitted by the MICU and/or night float resident with an appropriate note and orders, with the management plan developed in conjunction with the Team L attending on call. All patients must be staffed with Team L attending.
- Cross Coverage
- The Team L patients will be signed out to MICU and night float by one of the AP staff or Team L fellow on behalf of the entire team, with similar sign out to the faculty attending at 6:00 PM.
- Patients on Team L needing acute management will be covered after 6:00 PM until 7:00 AM by the night float and MICU teams until further notice. It is expected that the Attending and/or Heme/Onc Fellow will be actively available throughout this time to answer questions, facilitate in diagnosis and management, and come in to evaluate patients if needed.
- The nursing staff will be instructed to contact the NP/AP or Fellow during regular business hours M-F (0700 to 1800) for questions regarding the respective assigned patients.
- The nursing staff will be instructed to page the night float/MICU team for emergency situations requiring immediate physician evaluation and intervention, outside of regular business hours (0700 to 1800.
- The nursing staff will be instructed to page/contact the Team L Faculty Attending for routine questions/concerns/orders/responses to laboratory determinations, etc. from 1800 to 0700, 7 days a week.
- During weekend days, regular business hours (0700 to 1800), a clinical fellow will be available “on call” for Team L until such time as the full compliment of APs are in place.
- Daily Workflow
- Team L will have “working rounds” that, 1) start at 8:30 AM, 2) include the nurse assigned to each patient, and 3) incorporate multidisciplinary discharge rounds between 10:30 and 11:00.
- The Team L attending will be responsible for the distribution of patient assignments, to be distributed equitably between members of the team (advanced practitioner, faculty attending, and/or clinical Fellow).
- All clinics will be blocked for Team L Attending faculty, as the Attending is required to be physically available to the advanced practitioners during regular business hours M-F (0700 to 1800).
Team S Policies
- Admission Criteria
- All patients with documented malignancies that are non-hematologic in origin will be assigned to one of the Internal Medicine (Hospitalist) teams or other non-Team L services.
- Patients with a presumptive diagnosis of neoplasm, hematologic or nonhematologic, will be assigned to one of the Internal Medicine (Hospitalist) teams or other non-Team L services.
- Team S will function as a consult service for these patients.
- If and when a diagnosis is established for a hematologic malignancy, the patient can then be transferred to Team L, with Team L attending approval.
- Hematology/Oncology patients presenting to the ED and requiring admission will be triaged through the Team S fellow for possible admission to Team L (see above) or to another inpatient service.
- Inpatient Chemotherapy
- Chemotherapy for patients with non-hematologic malignancies, if needed as an inpatient, will be overseen by the Team S fellow and attending being comanaged with the primary attending service (guidelines below):
- a. Team S will be responsible for writing and submitting the orders for and the coordination of the administration of chemotherapy.
- b. This includes, all premedications, anti-emetics, IV fluids, and post chemotherapy growth factors if needed
- c. Team S will document the specifics and details of the chemotherapy regimen, inclusive of issues (toxicities or complications) to be aware of within the body of their consult progress note.
- d. Team S will meet with the Medicine team and provide chemotherapy education, specific to the chemotherapy regimen and general principles of management of patients receiving chemotherapy.
- e. Team S will provide a schedule for laboratory and radiographic monitoring and will be available for questions from the primary team.
- The administration of chemotherapy will require coordination with chemotherapy certified nursing staff (likely from 76/78) and/or relocation of the patient to 76/78, depending upon bed and staffing availability.
- Daily Workflow
- The usual PBG and Medical Staff requirements for timely consults and professional, timely communication will be enforced.
- Team S faculty will have either their AM or PM clinics blocked to facilitate timely and productive interactions with the admitting teams.
- It is the expectation that in-person communication and education will occur with the team during or juxtaposed to the Hospitalist Team rounds.
- Patients with established diagnosis of hematologic malignancies who are admitted to other services besides Team L may be staffed by the Team L attending in conjunction with the Team S fellow.
- Team L and Team S attendings are expected to coordinate their “rounds” with the Team S consult fellow.
- The Team S fellow, or similarly assigned “on call” clinical fellow, will remain “on call” for outpatient calls through the call center, after hours, regardless of patient diagnosis.
- It is the expectation that the Team S fellow will maintain communication with individual patient’s outpatient faculty attending throughout the course of their hospitalization.
D. Orthopedics
Last Updated: 03/01/2013
- Admission Criteria (applies only to elderly patients with fractures)
- Trauma Surgery
- >=60years with multiple trauma, including orthopedic injuries, with Orthopedics consult
- Medicine Consult service (Team H) may be consulted, as necessary, for management of medical issues
- Hospital Medicine
- >=60yrs with fractures without other traumatic injuries, with Orthopedics consult
- Admission Workflow
- Orthopedics will evaluate patients in ED and perform appropriate evaluation and splinting
- For operative candidates, Medicine (either primary hospitalist service or Team H) will perfrom appropriate medical workup and medically optimize patient, as appropriate.
- Patients admitted to Hospitalist service overnight will undergo preoperative evaluation by night float resident. Night float resident will staff preoperative recommendations with ICU nocturnist
- Once optimized, Orthopedics will perform surgery within 24 hours
- Orthopedics will be responsible for arranging followup for all patients. Follow up appointments, wound care and activity restrictions should be noted in discharge instructions and summary by Orthopedics team.
II. Rotation Logistics
Schedules
A. Rotation Schedule
- During three week night float block, residents will be assigned to admitting shifts for two weeks, and cross-cover for one week
- Admitting and cross-coverage assignments are listed on the Ward Call Schedule
B. Day Off Policy
- Days off are assigned for rotation. All night float residents will work Sunday night to Thursday night. Residents will be post-call on Friday, and off on Saturady
- Friday and Saturday night shifts will be covered by jeopardy and elective residents
Night Float Logistics
A. Back-Up Assistance
- The following sources can be used for backup assistance as needed:
- MICU night float team: MICU resident can assist with admissions, as needed
- CDDC Nocturnist: CDDC nocturnist can be contacted to assist with admissions. Nocturnist can be contacted via pager (p0890)
- Backup Resident: Senior resident on backup can be called in to assist with admissions. Backup resident should only be utilized if additional assistance still needed after other backup sources have been utilized. Resident should contact on-call chief resident.
- Medicine nocturnist is in-house and can be contacted if assistance is needed.
- Primary roles and responsibilities:
- Focus is on safety and quality of care for ALL medicine patients (emphasis on ICU), but also has responsibilities to the general medicine night float, including:
- Directly supervise MICU/CCU residents.
- Personally evaluate each new admission to the CCU and MICU.
- Supervise all of the following procedures: central line insertion, arterial line insertion, thoracentesis, paracentesis, lumbar puncture for both ICU AND Medicine ward patients.
- Additional responsibilities:
- Provide assistance to ward night float residents. Assistance may include anything the Nocturnist feels is appropriate- even taking over some of the work for the resident if the Nocturnist feels that is needed to avoid problems with quality of care or safety.
- Directly supervise medicine ward residents when necessary. If the Medicine Night Float resident calls for help for any reason, the Nocturnist is to provide assistance.
- Nocturnist is NOT:
- The Nocturnist is NOT the leader of the Code Blue Team. This remains the role of the MICU senior resident. In many situations, the Nocturnist should attend a Code Blue, but is not required to do so.
- The Nocturnist is NOT the admitting attending for general medicine ward patients or for ICU patients, and should not be listed as the cosigner on H&P's.
- The Nocturnist is NOT the on-call medicine consult attending. However, Nocturnists with faculty appointments have discretion to get involved with urgent medicine consults, if appropriate.
- The Nocturnist is NOT the in-house resident backup for completing work on stable patients. If the floor medicine residents call for assistance, the Nocturnist should make a sincere effort to investigate and determine if/how the Nocturnist's involvement can best help the situation, being professional in all interactions. This may include assistance with triage, helping residents prioritize their work, stabilizing situations, helping with admissions, calling in resident backup, or whatever assistance the Nocturnist feels is most appropriate to prevent safety or quality problems. Helping residents complete non-urgent work must never compromise the Core Responsibilities and Expectations.
B. Food
- Cafeteria: Open until 6:00AM-12:30AM daily, accept FreedomPay
- Vending machines: Located in ER waiting room, basement between Douglas Hospital and Tower
- Microwaves/Refrigerators: Available in nursing breakrooms, on all floors in Tower
C. Call Rooms
- Call rooms for ward night float residents available at:
- DH 3834: 3rd Floor, East Wing
- DH 5638: 5th Floor, adjcaent to Neurosciences SDU
- Sleep Trailer:
Building 58, Room 113 (keys located at T4 Nurses Station)
|
|



